Historically, the term fetal distress has been used to describe when the fetus does not receive adequate amounts of oxygen during pregnancy or labor. It is oftentimes detected through an abnormal fetal heart rate. However, while the term fetal distress is commonly used, it is not well defined. This makes it more difficult to make an accurate diagnosis and provide proper treatment. Because of the term’s ambiguity, its use has the potential to lead to improper treatment.
Fetal Distress: Diagnosis, Conditions & Treatment
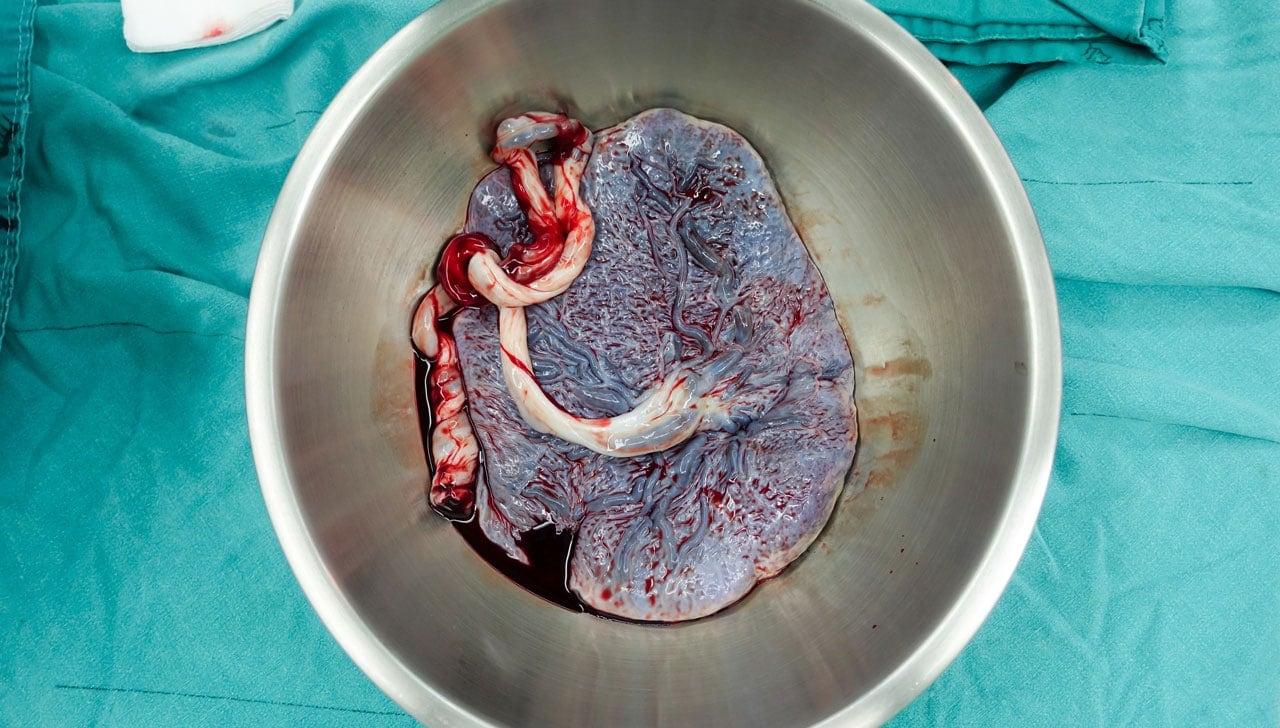
Fetal distress is commonly confused with the term birth asphyxia. Birth asphyxia occurs when the baby does not have adequate amounts of oxygen before, during, or after labor. This may have multiple causes, some of which include low oxygen levels in the mother’s blood or reduced blood flow due to compression of the umbilical cord.
As many have incorrectly used fetal distress and birth asphyxia as interchangeable terms, the Committee on Obstetric Practice of the American Congress of Obstetricians and Gynecologists (ACOG) has expressed concern regarding the use of the two terms. ACOG recommends that the term fetal distress be replaced with “non-reassuring fetal status.”
Along with this new term, ACOG further recommends physicians add to the diagnosis a list of additional findings such as fetal tachycardia, bradycardia, repetitive variable decelerations, low biophysical profile, and late decelerations. ACOG’s Committee on Obstetric Practice has also stated that the term birth asphyxia should no longer be used as it is too vague of diagnosis for medical use.
Fetal Distress Diagnosis
It is important for physicians to monitor the fetus throughout pregnancy to detect any potential complications. One of the more widely used methods of monitoring is electronic fetal heart rate (FHR) monitoring.
Benefits of FHR monitoring include:
- The ability to recognize the development of hypoxia (when the fetus does not receive adequate amounts of oxygen) by analyzing patterns in the fetal heart rate
- The ability to monitor the mother’s contractions
- The ability to monitor the response of the fetus to hypoxia
- A more positive outcome for high-risk deliveries
Nonetheless, FHR monitoring does come with risks as well, including an increased likelihood of having a cesarean section due to misinterpretation of FHR monitoring results.
Conditions Behind Fetal Distress
Potential precursors to fetal distress or non-reassuring fetal status may include:
- Anemia (the most prevalent obstetric condition seen behind non-reassuring fetal status)
- Oligohydraminos (a condition in which there is a lower level of amniotic fluid around the fetus)
- Pregnancy Induced Hypertension (PIH)
- Post-term pregnancies (42 weeks or more)
- Intrauterine Growth Retardation (IUGR)
- Meconium-stained amniotic fluid (a condition in which meconium, a baby’s first stool, is present in the amniotic fluid which can block fetal airways)
Treatment
The primary treatment used for non-reassuring fetal status is intrauterine resuscitation. This will help prevent any unnecessary procedures.
Some means of intrauterine resuscitation include:
- Changing the mother’s position
- Ensuring the mother is well-hydrated
- Ensuring the mother has adequate oxygen
- Amnioinfusion (the insertion of fluid into the amniotic cavity to alleviate compression of the umbilical cord)
- Tocolysis (a therapy used to delay preterm labor by temporarily stopping contractions)
- Intravenous hypertonic dextrose
Nonetheless, there are cases in which an emergency cesarean section is necessary. However, due to the over-diagnosis of fetal distress and potential misinterpretation of the fetal heart rate, it is recommended to confirm a potential fetal distress diagnosis with a fetal blood acid-base study. Overall, this condition points to the importance of prenatal care and proper monitoring of the mother and fetus throughout pregnancy.
Want to Know More?
Compiled from the following References:
ACOG Committee on Obstetric Practice. (2005). Inappropriate use of the terms of fetal distress and birth asphyxia. Committee Opinion, 326.
Beckmann, C. R. B., Ling, F. W., Barzansky, B. M., Herbert, W. N. P., Laube, D. W., & Smith, R. P. (2010). Obstetrics and gynecology (6th ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Bucklin, B. A., Gambling, D. R., & Wlody, D. J. (2009). A practical approach to obstetric anesthesia. Gravlee, G. P. (Ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Kaur, J., & Kaur, K. (2012). Conditions behind fetal distress. Annals of Biological Research, 3(10). Retrieved from https://scholarsresearchlibrary.com/ABR-vol3-iss10/ABR-2012-3-10-4845-4851.pdf
Mayo Clinic. (2012). Biophysical profile: Why it’s done.
Merck Manuals. (n.d.) Fetal distress.
The American Congress of Obstetricians and Gynecologists (ACOG). (2013, October 22). Ob-gyns redefine the meaning of “term pregnancy.”
University of California San Francisco Benioff Children’s Hospital. (n.d.). Birth asphyxia. Retrieved from https://www.ucsfbenioffchildrens.org/conditions/birth_asphyxia/